Xe-129 Hyperpolarized Gas: Revolutionizing Pulmonary MRI with 50,000x Signal Enhancement
BY Tao, Published Aug 15, 2025
The advent of Xe-129 hyperpolarized gas has marked a transformative era in pulmonary magnetic resonance imaging (MRI). With its ability to amplify MRI signals by up to 50,000 times, this noble gas isotope offers unparalleled insights into lung function, overcoming the limitations of traditional imaging modalities. As a nuclear research expert with over two decades of experience in rare gases, isotopes, and their applications, I have witnessed how Xe-129 is reshaping respiratory diagnostics. This article explores the science, applications, and practical considerations of Xe-129 hyperpolarized gas, presenting its revolutionary impact in a clear, authoritative, and accessible manner.
The Science Behind Xe-129 Hyperpolarization
Overcoming the Challenges of Lung Imaging
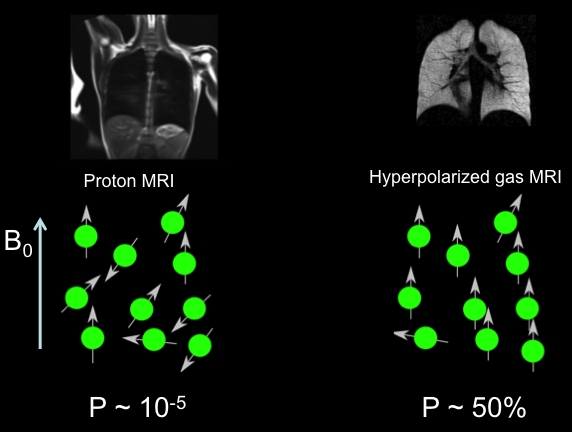
Lungs pose a unique challenge for MRI due to their low proton density, constant motion from breathing, and air-tissue interfaces that disrupt signal coherence. Conventional MRI, which relies on hydrogen protons in water, struggles to produce clear images of the lung’s airy structure. Xe-129 hyperpolarized gas addresses this by leveraging the nuclear spin properties of xenon-129, a stable isotope of the noble gas xenon. Through a process called spin-exchange optical pumping, the nuclear spins of Xe-129 atoms are aligned far beyond their thermal equilibrium state, resulting in a magnetic resonance signal amplified by 10,000 to 50,000 times.
How Hyperpolarization Works
Spin-exchange optical pumping involves exposing Xe-129 gas to circularly polarized laser light in the presence of an alkali metal vapor, typically rubidium. The laser polarizes the rubidium electrons, which then transfer this polarization to the xenon nuclei through collisions. This process achieves polarization levels of 38-54% for a 250 mL xenon volume, compared to the 0.0001% alignment in standard MRI fields. The hyperpolarized state is transient, with a T1 relaxation time of minutes, necessitating on-site preparation and immediate use. Once inhaled, Xe-129 resonates at distinct chemical shifts—0 ppm in the gas phase, 197 ppm in tissue/plasma, and 217 ppm in red blood cells—enabling multi-compartment imaging of ventilation and gas exchange.
Evolution from Helium-3
Hyperpolarized gas MRI began with helium-3, valued for its high gyromagnetic ratio and safety. However, helium-3’s scarcity, derived from tritium decay in nuclear stockpiles, made it prohibitively expensive. Xe-129, with a natural abundance of 26% (enrichable to >80%), emerged as a viable alternative by the early 2000s. Advances in laser technology and gas mixture optimization have brought Xe-129’s signal strength close to helium-3’s, making it the preferred choice for clinical applications, as evidenced by its FDA approval for pulmonary MRI.
Clinical Applications of Xe-129 Hyperpolarized Gas
Ventilation Imaging
The primary application of Xe-129 hyperpolarized gas is ventilation imaging, where patients inhale a dose during a breath-hold scan. The resulting high-resolution images, achievable in 10-15 seconds, map regional airflow distribution. In diseases like asthma or chronic obstructive pulmonary disease (COPD), ventilation defects appear as dark patches, indicating obstructed airways or destroyed alveoli. Unlike nuclear scintigraphy, this method avoids ionizing radiation, making it suitable for repeated use in sensitive populations, including children.
Gas-Exchange Imaging
Xe-129’s solubility in tissues and blood enables gas-exchange imaging, a breakthrough for assessing interstitial lung diseases. By tracking xenon diffusion across the alveolar-capillary barrier, clinicians can quantify membrane thickness and gas-transfer efficiency. In idiopathic pulmonary fibrosis, reduced signal in dissolved-phase maps signals thickened septa, while in post-COVID-19 lung damage, it reveals microvascular impairments. These insights are critical for early diagnosis and monitoring treatment efficacy.
Quantitative Metrics
Xe-129 MRI provides robust biomarkers for lung health:
- Apparent Diffusion Coefficient (ADC): Measures alveolar microstructure; elevated values (e.g., >0.1 cm²/s) indicate enlarged airspaces in emphysema.
- Ventilation Defect Percentage (VDP): Quantifies poorly ventilated lung regions; values >15% correlate with moderate-to-severe COPD.
- Gas-Exchange Ratios: Red blood cell-to-tissue ratios (normal: 0.3-0.5) detect impaired gas transfer in fibrotic or vascular diseases. These metrics surpass spirometry’s sensitivity, detecting abnormalities in up to 30% of smokers with normal lung function tests.
Key Clinical Indications
Xe-129 hyperpolarized gas excels in diverse scenarios:
- Asthma: Maps heterogeneous ventilation to guide biologics or bronchial thermoplasty.
- COPD: Differentiates emphysema from airway obstruction, aiding decisions on lung volume reduction surgery.
- Interstitial Lung Disease: Tracks gas-transfer deficits to monitor antifibrotic therapies.
- Pediatric Imaging: Safe for ages 6+, it evaluates congenital anomalies without sedation.
- Lung Transplantation: Detects early rejection or infection via regional perfusion mismatches.
Product Specifications and Performance
Composition and Preparation
Xe-129 hyperpolarized gas is supplied as a blend with nitrogen, prepared using systems like the HPX Hyperpolarizer. The gas is enriched to >80% Xe-129, with a polarization fraction of 38-54% for a 250 mL xenon volume. The dose equivalent (DE) ranges from 75-100 mL, calculated as DE = (xenon volume) × (enrichment fraction) × (polarization fraction). It is dispensed into a 1,000 mL delivery bag, containing 250-750 mL xenon diluted with nitrogen for safe inhalation.
Imaging Performance
At 1.5T or 3T MRI field strengths, Xe-129 delivers signal-to-noise ratios sufficient for 3D imaging with 3-5 mm resolution. In healthy lungs, ventilation maps show >90% coverage, while diseased lungs may drop below 80%. Gas-exchange imaging yields red blood cell-to-tissue ratios of 0.3-0.5 in healthy subjects, with deviations signaling pathology. Reproducibility is high, with longitudinal variation <5%, ideal for tracking disease progression or therapeutic response.
Administration and Precautions
The gas is inhaled in a single breath-hold via a mouthpiece, with patients holding their breath for 10-15 seconds. MRI scanners must be multi-nuclear capable, tuned to Xe-129’s resonance frequency (11.8 MHz at 1T). Key precautions include:
- Oxygen Management: Withhold supplemental oxygen for two breaths prior to inhalation to avoid signal loss from oxygen’s paramagnetic effects.
- Monitoring: Continuous pulse oximetry is required due to transient hypoxia risks from the anoxic gas mixture.
- Side Effects: Up to 20% of patients report transient dizziness, tingling, or euphoria, resolving within minutes.
- Contraindications: No absolute contraindications; caution in pregnancy due to limited data. The gas must be prepared fresh and used immediately, as polarization decays rapidly.
Product Details Table
| Aspect | Details |
|---|---|
| Composition | Hyperpolarized Xe-129 (>80% enrichment) blended with nitrogen. |
| Dose Equivalent | 75-100 mL; minimum 75 mL for efficacy. |
| Polarization | 38-54% for 250 mL xenon; signal enhancement 10,000-50,000x. |
| Administration | Single breath-hold (10-15s); 1,000 mL bag with 250-750 mL xenon. |
| Imaging | 1.5T/3T MRI; 3-5 mm resolution; multi-slice or 3D sequences. |
| Performance Metrics | Ventilation: >90% healthy; ADC: 0.05-0.1 cm²/s; gas-exchange ratio: 0.3-0.5. |
| Precautions | Monitor SpO2; withhold O2 pre-inhalation; not for perfusion imaging. |
| Side Effects | Transient: desaturation (5-10%), heart rate increase, numbness, euphoria. |
| Contraindications | Caution in pregnancy/breastfeeding; no absolute contraindications. |
| Storage/Preparation | Fresh preparation; use within minutes; requires hyperpolarizer. |
Challenges and Future Directions
Current Limitations
Despite its promise, Xe-129 hyperpolarized gas faces hurdles. Polarization equipment remains costly, though prices are dropping. The transient nature of hyperpolarization requires on-site production, limiting availability to specialized centers. Signal decay due to T1 relaxation (influenced by oxygen or field inhomogeneities) demands optimized protocols. Additionally, training radiologists to interpret dissolved-phase images is critical for widespread adoption.
Emerging Innovations
The future is bright, with advancements like low-field MRI systems enabling portable imaging and combined Xe-129/proton protocols enhancing anatomical-functional correlation. AI-driven image analysis is streamlining defect quantification, potentially integrating Xe-129 MRI into routine screenings. Research into hyperpolarized gas mixtures with other isotopes, like krypton-83, may further expand applications.
The Path Forward for Pulmonary Imaging
Xe-129 hyperpolarized gas is more than a contrast agent—it’s a window into the lungs’ functional dynamics. Its 50,000x signal enhancement illuminates ventilation and gas-exchange patterns with unmatched precision, offering hope for early detection and personalized treatment of respiratory diseases. As costs decrease and technology advances, this tool could become a cornerstone of pulmonary diagnostics, from clinical trials to community hospitals. With my decades-long perspective on noble gases, I see Xe-129 as a testament to how nuclear science can breathe new life into medical innovation, one inhale at a time.
Would you like a deeper dive into any specific technical parameters or applications?
(Follow up our update articles on www.asiaisotopeintl.com or send your comments to tao.hu@asiaisotope.com for further communications)